Lesson 25.1: Male Reproductive System
Lesson 25.1: Male Reproductive System
Lesson Objectives
Explain how the male reproductive system develops before birth and matures during puberty.
Identify structures of the male reproductive system and their functions.
Describe how sperm are produced and how they leave the body.
Introduction
The male reproductive system is a collection of organs and other structures in the pelvic region. Most of the structures are located outside the body. The male reproductive system has two major functions: producing sperm and secreting male sex hormones. Sperm are male gametes, or sex cells, which are necessary for reproduction. During puberty, a boy develops into a sexually mature male, capable of producing sperm and reproducing.
Sexual Development in Males
The main visible differences between boys and girls at birth are their reproductive organs. Of course, there are other differences between boys and girls at birth, but in this chapter, the focus is on their reproductive systems. As different as the male and female reproductive systems are at birth, they start out relatively similar. Before birth, the expression of genes on the male Y-chromosome brings about the differences.
Development Before Birth
In the first few weeks of life, male and female embryos are essentially the same, except for their chromosomes. Females have two X chromosomes, and males have an X and a Y chromosome. In male embryos, genes on the Y chromosome lead to the synthesis of testosterone. This begins around the sixth week of life.
Testosterone is a masculinizing hormone and the chief sex hormone in males. Testosterone stimulates the embryo’s reproductive organs to develop into male organs. For example, because of testosterone, the embryo develops testes instead of ovaries, which are female organs you will read about in Lesson 25.2.
All the reproductive organs are present by birth. However, they are immature and unable to function. The reproductive organs grow very little during childhood and do not mature until puberty.
Puberty and Its Changes
Puberty is the period during which humans become sexually mature. In the United States, boys generally begin puberty at about age 12 years. Puberty starts when the hypothalamus, a gland in the brain, stimulates the nearby pituitary gland to secrete hormones that target the testes. The main pituitary hormone responsible for puberty in males is luteinizing hormone (LH). It stimulates the testes to produce testosterone. Testosterone promotes protein synthesis and growth. It brings about most of the physical changes of puberty, including the changes outlined in Table 25.1.
Table 25.1: Changes in Males During Puberty
Changes in Reproductive Organs
Testes grow larger Penis grows longer
Other reproductive structures grow Sperm production begins
Other Physical Changes
Pubic hair grows Facial and body hair grow
Bone density increases Long bones grow Muscle mass and strength increase Bones in face grow
Adam’s apple grows Apocrine sweat glands develop
Shoulders widen Voice deepens
Cells that are targeted by testosterone are those that have testosterone receptors. Receptors are molecules in or on cells that bind to specific hormones. Testosterone receptors are on the nucleus of cells. After binding to testosterone, they enter the nucleus, where they bind to specific DNA sequences and regulate gene transcription.
Some of the changes in Table 25.1 involve maturation of the reproductive organs, including the penis. Traits such as adult penis size are called primary sex characteristics. Other changes, such as growth of pubic hair, are not directly related to reproduction. Character- istics of mature males such as pubic hair are called secondary sex characteristics.
Adolescent Growth Spurt
Another obvious change that occurs during puberty is rapid growth in height. This is called the adolescent growth spurt. In males, the rate of growth usually starts to increase relatively early in puberty. At its peak rate, growth in height is typically about 10 centimeters per year. Growth generally remains rapid for several years. Growth and development of muscles occur toward the end of the growth spurt in height. Muscles may continue to develop and gain strength after growth in height is finished.
Timing of Puberty
The ages at which particular changes of puberty occur differ from one person to another. However, the changes generally occur in the same sequence for most males. The sequence in which some of the more obvious changes occur is represented by the following stages:
Stage 1—The scrotum and testes grow larger.
Stage 2—The penis becomes longer; pubic hair appears.
Stage 3—Facial and underarm hair appear; the voice deepens.
In the U.S., the average boy begins Stage 1 of puberty at age 11.5 years. He begins the growth spurt in height by the second year of puberty, develops the ability to produce sperm a few years later, and continues to grow in height until age 17.5 years. Overall, he spends about six years going through puberty.
Depending on the genes he inherits, his diet, and many other factors, a boy may go through puberty a couple of years earlier or later than the average. This is usually normal, and early and late maturers generally have nothing to worry about. Nonetheless, a boy who is concerned that he is not developing normally should talk with his doctor.
Male Reproductive Organs
Penis, Testes, and Epididymis
The penis is an external genital organ with a long shaft and enlarged tip. It contains tissues that can fill with blood and cause an erection, which is stiffening and enlarging of the penis.
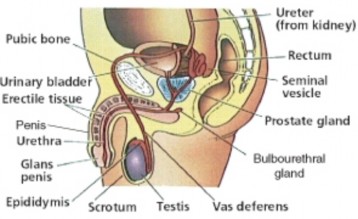
A duct called the urethra passes through the penis. Sperm pass out of the body through the urethra. (During urination, the urethra carries urine from the bladder.)
The testes (singular, testis) are located in the scrotum, which is a sac of skin between the upper thighs. By hanging away from the body, the testes keep sperm at a temperature lower than normal body temperature. The lower temperature is needed for sperm production.
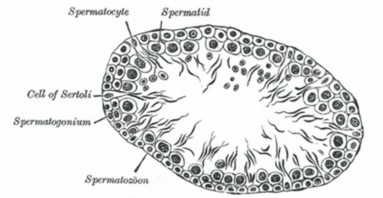
Each testis contains more than 90 meters of tiny, tightly-packed tubes called seminiferous tubules. They are the functional units of the testes, where sperm are produced and testos- terone is secreted. A cross-section of a seminiferous tubule is shown in Figure 25.2. The tubule is lined with spermatogonia and Sertoli cells. Spermatogonia are sperm-producing cells that you will read more about below. Sertoli cells help protect and nourish developing sperm.
In between the seminiferous tubules in the testes are interstitial cells, also called Cells of Leydig. These cells secrete testosterone. A high concentration of testosterone is necessary for sperm production. Testosterone is also needed throughout a man’s life to maintain his secondary sex characteristics.
The seminiferous tubules join together to form the epididymis. The epididymis is a coiled tube about 6 meters long lying atop the testes inside the scrotum (Figure 25.1). Its functions are to help sperm mature and to store mature sperm until they leave the body.
Ducts and Glands
In addition to these organs, the male reproductive system consists of a series of ducts and glands. These are also shown in Figure 25.1.
Ducts include the vas deferens and ejaculatory ducts. They transport sperm from the epididymis to the urethra in the penis.
Glands include the seminal vesicles, prostate gland, and bulbourethral glands. They secrete substances that become part of semen.
Semen is the fluid that is ejaculated from the urethra. Semen contains secretions from the glands as well as sperm. The secretions control pH and provide the sperm with nutrients for energy.
Production and Delivery of Sperm
A sexually mature male typically produces several hundred million sperm per day. Sperm production usually continues uninterrupted until death, although the number and quality of sperm decline during later adulthood.
Spermatogenesis
Spermatogenesis is the process of producing mature sperm. Sperm are haploid cells, mean- ing they have half the number of chromosomes as other cells of the body, which are diploidcells. Sperm must be haploid in order for normal sexual reproduction to occur. During reproduction, a sperm unites with another cell, called an egg. This is called fertilization. Unless both sperm and egg are haploid, the resulting offspring will not have the diploid number of chromosomes (see chapter titled Cell Division and Reproduction).
Sperm are produced in the seminiferous tubules of the testes and finish maturing in the epididymis. The entire process takes about 9 to 10 weeks. As shown in Table 25.2, the production of sperm occurs in several steps, each involving a different type of cell and process.
Spermatogenesis begins when a spermatogonium with the diploid number of chromosomes undergoes mitosis to form primary spermatocytes, also with the diploid number. It proceeds as a primary spermatocyte undergoes the first cell division of meiosis to form secondary sper- matocytes with the haploid number of chromosomes. A secondary spermatocyte undergoes the second meiotic cell division to form haploid spermatids. Spermatids mature into sperm, which are also haploid.
Table 25.2: Spermatogenesis and Cell Division
|
Type of Cell |
Number of Chromosomes |
Process |
|
Spermatogonium |
Diploid |
Mitosis |
|
Primary Spermatocyte |
Diploid |
Meiosis 1 |
|
Secondary Spermatocyte |
Haploid |
Meiosis 2 |
|
Spermatid |
Haploid |
Maturation |
|
Spermatozoon (sperm) |
Haploid |
Fertilization |
Spermatogonia, which line the seminiferous tubules in the testes, are diploid cells. They begin the process of spermatogenesis when they divide by mitosis to produce cells called primary spermatocytes, which are also diploid cells. Some spermatogonia divide just to produce copies of themselves. This ensures a constant supply of spermatogonia for future sperm production.
Primary spermatocytes go through the first cell division of meiosis to produce secondary spermatocytes. These are haploid cells. Secondary spermatocytes then quickly complete the meiotic division to become spermatids, which are also haploid cells.
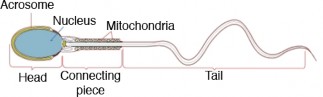
Spermatids slowly mature into sperm, like the one shown in Figure 25.3. Among other changes, they lose excess cytoplasm from the head and grow a tail. The tail is a flagellum that lets them move by rotating like a propeller. The acrosome that covers part of the head produces digestive enzymes that help the head penetrate an egg. The mitochondria in the connecting piece produce energy that the sperm needs to “swim” through the female reproductive tract to reach an egg. However, sperm do not develop the ability to move until they complete their maturation in the epididymis. It takes sperm four to six weeks to travel through the epididymis and become fully mature. After they mature, they remain in the epididymis until they leave the body.
Ejaculation
In order for reproduction to take place, sperm must leave the reproductive system. Sperm are released from the body during ejaculation. About 200 to 500 million sperm are released with each ejaculation. Ejaculation occurs when rhythmic muscular movements of the vas deferens propel sperm from the epididymis. The sperm are forced through the vas deferens and ejaculatory ducts and out of the body through the urethra. As sperm travel through the ducts, they mix with fluids from the seminal vesicles, prostate gland, and bulbourethral glands to form semen.
Lesson Summary
The male reproductive system forms before birth but does not become capable of reproduction until it matures during puberty.
The male reproductive system includes organs and other structures that produce sperm and deliver sperm and secrete testosterone.
Sperm are produced in the testes in the process of spermatogenesis and leave the body through the penis during ejaculation.
Review Questions
Further Reading / Supplemental Links
What are the two major functions of the male reproductive system?
List four physical changes that occur in males during puberty.
Name two male reproductive organs and identify their functions.
Describe how sperm leave the body.
Sexual dimorphism refers to differences between males and females of the same species. Based on what you read in this lesson, how does human sexual dimorphism change from birth to adulthood?
If a man did not have an epididymis, how would this affect his ability to produce mature sperm?
Make a flow chart showing the steps of spermatogenesis. Indicate the cells and process involved at each step.
What are the roles of testosterone in the male reproductive system, from the embryo to old age?
Stanley, Deborah, Sexual Health Information for Teens. Omnigraphics, 2003.
Walker, Pam and Wood, Elaine, Understanding the Human Body: The Reproductive System. Lucent Books, 2002.
http://en.wikibooks.org/wiki/Human_Physiology/The_male_reproductive_system
http://www.kidshealth.org/parent/general/body_basics/male_reproductive.html
http://www.kidshealth.org/teen/sexual_health/changing_body/male_repro.html
http://www.medicalook.com/human_anatomy/systems/Male_Reproductive_System. html
Vocabulary
acrosome Covers part of the sperm cell head; produces digestive enzymes that help the sperm head penetrate an egg.
adolescent growth spurt Rapid growth in height seen during puberty.
Cells of Leydig Cells that secrete testosterone, located in between the seminiferous tubules in the testes; are also known as interstitial cells.
epididymis A coiled tube about 6 meters long lying atop the testes inside the scrotum; helps sperm mature and stores mature sperm until they leave the body.
fertilization The uniting of a haploid sperm with a haploid egg.
luteinizing hormone The main pituitary hormone responsible for puberty in males; stim- ulates the testes to produce testosterone.
male reproductive system System with two major functions: producing sperm and se- creting testosterone.
primary sex characteristics Traits of reproductive organs seen in mature adults that are directly related to reproduction.
puberty The period during which humans become sexually mature.
secondary sex characteristics Physical traits of mature adults which are not directly related to reproduction.
semen The fluid that is ejaculated from the urethra; contains sperm and secretions from the seminal vesicles, prostate gland, and bulbourethral glands.
seminiferous tubules The functional units of the testes, where sperm are produced and testosterone is secreted.
sertoli cells Help protect and nourish developing sperm, located in the seminiferous tubules. sperm Male gametes, or sex cells, which are necessary for reproduction; haploid. spermatogonia Sperm-producing cells, located in the seminiferous tubules; diploid. spermatogenesis The process of producing mature sperm.
testosterone A masculinizing hormone and the chief sex hormone in males.
Points to Consider
By the time they finish puberty, males have developed the traits of mature adults of their own sex. They differ from mature females in many ways. How do these differences between sexually mature males and females come about?
What causes female to develop differently during puberty?
When do girls begin puberty, what changes do they go through, and what hormones control the changes?
- Log in or register to post comments
- Email this page
